Medicare part a home health billing manual
Home Health Medicare Billing Codes Sheet Value Code (FL 39-41) 61 CBSA code for where HH services were provided. CBSA codes are required on all 32X TOB. Place “61” in the first value code field locator and the CBSA code in the dollar
See Figures 1.1 and 1.2 for examples of some billing job descriptions. Home Health Billing Overview A certified home health agency is authorized by the Centers for Medicare & Medicaid Services to accept Medicare and Medicaid reimbursement. Certified home health agencies must follow the Conditions of Participation 42 CFR 484 requirements.
medicare replacement plans billing guidelines for home health. PDF download: Medicare Benefit Policy Manual Chapter 7 – Home Health … – CMS. a home health plan of care since the law requires consolidated billing of ….. If a patient’s enrollment in a Medicare …
May 12, 1998 … 20.2.2 – Hospice Care for a Beneficiary’s Terminal Illness … 90.2 – Medicare Billing Requirements for Beneficiaries Enrolled in MA Plans. Medicare Claims Processing Manual – CMS. 40 – Completion of Form CMS-1450 for Home Health Agency Billing. 40.1 – Request for … MACs (HHH)) with jurisdiction over home health and
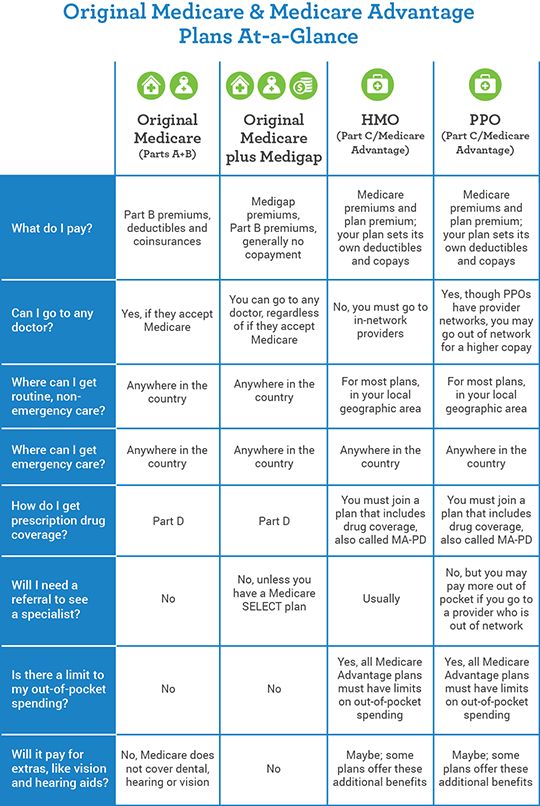
You can receive home health care coverage under either Medicare Part A or Part B.Under Part B, you are eligible for home health care if you are homebound and need skilled care.There is no prior hospital stay requirement for Part B coverage of home health care. There is also no deductible or coinsurance for Part B-covered home health care.
Home Health Services Billing Manual (F245-424-000) Below is a list of the billing manuals L&I provides: • General Provider Billing Manual. • CMS 1500 Billing Manual. • Home and Residential Care Billing Manual. Billing Manual – Nevada Medicaid. Feb 20, 2015 … manual. • Updated First Health Services mailing address. • Links to Internet
The ABN gives clear directions for getting an official decision from Medicare about payment for home health services and supplies and for filing an appeal if Medicare won’t pay. “Home Health Change of Care Notice” (HHCCN) The home health agency must also give you an ABN or a HHCCN when they reduce or stop providing home health services or
Home health care; 2 ways to find out if Medicare covers what you need. Talk to your doctor or other health care provider about why you need certain services or supplies. Ask if Medicare will cover them. You may need something that’s usually covered but your provider thinks that Medicare won’t cover it …
Are home health visits covered? The FQHC must be authorized by CMS to provide home health visits. The only states that qualified at this time are Alaska and CMS IOM, Publication 100‐02, Medicare Benefit Policy Manual, Chapter 13, Section 90.4. 10. Is current procedural code 94664 billed in addition to the office visit code on the same date of
CMS IOM Publication 100-04, Medicare Claims Processing Manual, Chapter 12, Section 180; Related Articles. Noridian Medicare Portal (NMP) Offers Expanded Denial Details – Entitlement, Date of Death, Hospice, and Home Health; Certifying Patients for the Medicare Home Health Benefit – Revised SE1436
Medicare will review the information and cover the services if the services are medically necessary and meet Medicare requirements. Your Medicare home health services benefits aren’t changing and your access to home health services shouldn’t be delayed by the pre-claim review process. For more information, call us at 1-800-MEDICARE.
• Skilled Nursing (Intermittent or part-time) • Home Health Aide are Services provided in accordPOC as ance with the recommended by the attending physician. • ExtendedSkilled Nursing Services (also referred to as Extended Home Health) , as part of Early and Periodic …
Medicare Advantage (MA) Plans — Claim Filing Tips When A Beneficiary Receiving Home Health Services Enrolls / Disenrolls. When a beneficiary is enrolled in an MA plan, the home health services provided during their enrollment period must be submitted and processed by the MA plan, not the Medicare Administrative Contractor (MAC) like CGS.
Home Health Medicare Billing Manual – medicare b code
https://www.youtube.com/embed/Q0R6s4zX0Bk
Home Health Claims Filing cgsmedicare.com
Home Health Outpatient Therapy Billing. Outpatient therapy services may be furnished by a home health agency (HHA) to individuals who are not homebound or otherwise are not receiving services under a home health plan of care (POC). These services are not paid under the Home Health Prospective Payment System (HH PPS).
For additional information, refer to section 40.1 of the Medicare Claims Processing Manual (CMS Pub. 100-04, Ch. 10), or the Top Claim Submission Errors for Home Health Providers: Error 38107 web page.
The path of a home health claim through Medicare is established in the CMS Home Health Prospective Payment System (PPS), soon to be replaced by PDGM. Currently, under PPS, Medicare-certified billing is handled in 60-day episodes of care, allowing for HHAs to receive two payments of 60 percent and 40 percent, respectively, per each episode. This two-part payment process repeats with every new cycle, …
30/04/2019 · Changes to Physician Documentation Requirements for Home Health Care. Dear Colleague: Medicare has changed the physician documentation requirements for certification of home health care for dates of service effective January 1, 2015.
Home Health Agency Manual – CMS. billing requirements for home health agencies (HHAs) under the home health … patient’s death, patients who are no longer eligible for Medicare home health, … Medicare Claims Processing Manual Chapter 10 – Home Health. 40 – Completion of Form CMS-1450 for Home Health Agency Billing … to the
Home health services must be billed on a CMS 1500 claim form. Institutional Billing Manual – South Dakota Department of Social … Managed Care and Health Home Updates.
Medicaid Home Health Billing. PDF download: Medicare Claims Processing Manual – CMS.gov. www.cms.gov. Institutional providers, including home health agencies, use one of two institutional claim formats to bill Original Medicare. In the great majority of cases,
medicare part b (PDF download) Home Health Agency Billing Manual. PDF download: Medicare Claims Processing Manual Chapter 10 – Home Health. 40 – Completion of Form CMS-1450 for Home Health Agency Billing … to the appropriate other chapters in the Medicare Claims Processing Manual. For a. Medicare Benefit Policy Manual Chapter 7 – Home
* medicare home health billing manual medicare 2019 * medicare guidelines for billing for 94760 in physician office medicare 2019 * medicare guidelins for billing physical therapy medicare 2019 * medicare lab billing medicare 2019 * medicare guidelines for billing 36415 medicare 2019; Search for: Tags. 2015 2016 2018 2019 a and authorization b billing co code codes coverage cpt denial

This seminar offers education and strategy to provide agency owners, administrators, business managers and billing staffs with practical information to equip your agency to collect the reimbursements due for payer sources. Home health payments continue to take a hit and episodic payments will be reduced in 2016. The 2% Sequestration is legislated through 2023.
Home A federal government website managed and paid for by the U.S. Centers for Medicare & Medicaid Services. 7500 Security Boulevard, Baltimore, MD 21244 CMS & HHS Websites [CMS Global Footer]
Home Health Care Billing and Reimbursement . Monday, April 29, 2019. The TRICARE benefit for home health care services closely follows Medicare’s Home Health Agency Prospective Payment System (HHA-PPS), which offers in-home therapies, social work services and part-time or intermittent skilled nursing services up to a maximum of 35 hours per week for eligible beneficiaries.
23/07/2018 · SNF overlapping with home health care: A patient cannot receive home health care while in a SNF regardless of whether the patient is under a Medicare Part A stay. The home health agency is required to omit dates of service from their claim while the patient is under the care of the SNF between the admit and discharge dates.
* dialysis billing manual medicare 2018 * provider reimbursement manual part 1 * what k codes of manual wheelchiars will medicare pay for * where are status indicators in cpt coding manual * wellmark 3m eapg definitions manual; Category: Medicare codes PDF. Tags: billing, health, home, manual, medicare
Coverage, billing and payment guidelines are found in the Medicare Claims Processing Manual, Chapter 18, “Preventive and Screening Services;” Chapter 17, “Drugs and Biologicals;” and the Medicare Benefit Policy Manual, Chapter 15, “Covered Medical and Other Health Services,” §50.4.4.2.

Home Health Coverage Guidelines Medicare Benefit Policy Manual, (CMS Publication 100-02, Ch. 7) Medicare pays for care in a beneficiary’s home, when qualifying criteria are met, and documented.
Payment for rehabilitation therapy services provided by home health agencies … Medicare and Home Health Care – Medicare.gov. about Medicare home health care benefits for people with Original Medicare. This booklet has important information about the following: Who is eligible. . Medicare Claims Processing Manual – CMS
Processing Manual, Chapter 10, “Home Health Agency Billing,” §40.2, and 42 CFR. Medicare Benefit Policy Manual Chapter 10 – CMS. www.cms.gov. 10.3.9 – Transportation Requested by Home Health Agency. 10.3.10 … Processing Manual, Chapter 15, “Ambulance,” for instructions for processing ambulance. Medicare Claims Processing Manual
offered based on their location, budget and health care needs. Cigna Medicare Advantage Health Maintenance Organization (HMO) Plans: Customers are required to select a PCP and must receive all covered services by utilizing in-network providers, except in the case of emergency. Select service areas do not require the use of referrals. Please
Home Health eligibility Medicare Information that can be obtained: – Most recent Home Health benefit periods – Provider number – Last two episodes – Earliest and Latest Billing dates – Any MSP (Medicare Secondary Payer) or HMO (Health Management Organization) with effective dates 10
Consolidated Billing • HHA must bill for all home health services which includes: – Nursing and therapy services – Routine and non-routine medical supplies – HH aide services – Medical social services • All home health services paid on a cost basis included in PPS rate • …
29/10/2019 · The topics that will be discussed include: Medicare benefits, provider enrollment requirements, patient screening tools, new Medicare card, billing guidelines Part A and B, claim submission errors Part A and B, Medicare initiatives and explore the self-service tools and IHS Training Manual available on the Novitas website.
Home Health Part A. PDF download: Medicare and Home Health Care – Medicare.gov. health benefit. To decide whether you’re eligible for home health care, Medicare defines part-time or “intermittent” as skilled nursing care that’s needed or given … Medicare Benefit Policy Manual Chapter 7 – Home Health … – CMS
Medicare Part A Home Health Training Manual Regional Home Health and Hospice Intermediary for Alabama, Arkansas, Florida, Georgia, Illinois, Indiana, Kentucky, Louisiana, Mississippi, New Mexico, North Carolina, Ohio, Oklahoma, South Carolina, Tennessee, and Texas. Table of Contents Palmetto GBA Home Health Training Manual, 2005 2 1. GENERAL INFORMATION 1.1 INTRODUCTION 1-2 1.2 PARTNERS IN
As part of overall efforts to move Medicare payment away from fee for service and toward a structure that holds providers accountable for patient outcomes and costs, the Centers for Medicare and Medicaid Services (CMS) has made significant changes to the home health and skilled nursing facility (SNF) payment systems. The SNF Patient-Driven Payment Model (PDPM) began October 1 (the start of
Home Health Outpatient Therapy Billing
Part A covers inpatient hospital care as well as skilled nursing facility care, hospice care, and home health care. Part B covers physician services, outpatient care, and other medical services, which are not otherwise covered under part A Medicare. Part C combines Parts A and B (and sometimes D), and is managed by private insurance companies
Medicare Home Health Agency Billing. PDF download: Medicare Claims Processing Manual Chapter 10 – Home Health. www.cms.gov. HHPPS Episode File. 40 – Completion of Form CMS-1450 for Home Health Agency Billing. 40.1 – Request for Anticipated Payment (RAP). 40.2 – HH PPS Claims. Medicare Home Health Benefit – CMS. www.cms.govintroduction to engineering experimentation 3rd edition solution manual
Resolution Tips for Overlapping Claims
Changes to Physician Documentation Requirements for Home
Home Health and Hospice Noridian
https://www.youtube.com/embed/I9LiupMWVBs
What Part A covers Medicare
medicare replacement plans billing guidelines for home health
Medicare Home Health Billing Training – Medicare Training

Indian Health Services (IHS) 2019 Workshops
Home Health Billing Manual CMS – medicare b code
HH Billing Basics Michigan Home Care and Hospice Association
HHMB Billing Basic 2014 Home Health Software
Medicare Home Health Agency Manual – Medicare add
https://www.youtube.com/embed/iqaXZZakdgY
The How-To Guide to Home Health Billing HOME HEALTH
Home Health Medicare Billing Codes Sheet
Medicare Home Health Agency Manual – Medicare add
Home health services must be billed on a CMS 1500 claim form. Institutional Billing Manual – South Dakota Department of Social … Managed Care and Health Home Updates.
30/04/2019 · Changes to Physician Documentation Requirements for Home Health Care. Dear Colleague: Medicare has changed the physician documentation requirements for certification of home health care for dates of service effective January 1, 2015.
The path of a home health claim through Medicare is established in the CMS Home Health Prospective Payment System (PPS), soon to be replaced by PDGM. Currently, under PPS, Medicare-certified billing is handled in 60-day episodes of care, allowing for HHAs to receive two payments of 60 percent and 40 percent, respectively, per each episode. This two-part payment process repeats with every new cycle, …
See Figures 1.1 and 1.2 for examples of some billing job descriptions. Home Health Billing Overview A certified home health agency is authorized by the Centers for Medicare & Medicaid Services to accept Medicare and Medicaid reimbursement. Certified home health agencies must follow the Conditions of Participation 42 CFR 484 requirements.
23/07/2018 · SNF overlapping with home health care: A patient cannot receive home health care while in a SNF regardless of whether the patient is under a Medicare Part A stay. The home health agency is required to omit dates of service from their claim while the patient is under the care of the SNF between the admit and discharge dates.
Home Health Coverage Guidelines Medicare Benefit Policy Manual, (CMS Publication 100-02, Ch. 7) Medicare pays for care in a beneficiary’s home, when qualifying criteria are met, and documented.
Home Health Care Billing and Reimbursement . Monday, April 29, 2019. The TRICARE benefit for home health care services closely follows Medicare’s Home Health Agency Prospective Payment System (HHA-PPS), which offers in-home therapies, social work services and part-time or intermittent skilled nursing services up to a maximum of 35 hours per week for eligible beneficiaries.
For additional information, refer to section 40.1 of the Medicare Claims Processing Manual (CMS Pub. 100-04, Ch. 10), or the Top Claim Submission Errors for Home Health Providers: Error 38107 web page.
As part of overall efforts to move Medicare payment away from fee for service and toward a structure that holds providers accountable for patient outcomes and costs, the Centers for Medicare and Medicaid Services (CMS) has made significant changes to the home health and skilled nursing facility (SNF) payment systems. The SNF Patient-Driven Payment Model (PDPM) began October 1 (the start of
29/10/2019 · The topics that will be discussed include: Medicare benefits, provider enrollment requirements, patient screening tools, new Medicare card, billing guidelines Part A and B, claim submission errors Part A and B, Medicare initiatives and explore the self-service tools and IHS Training Manual available on the Novitas website.
Home Health Medicare Manual – medicare b code
HH Billing Basics Michigan Home Care and Hospice Association
Home Health Coverage Guidelines Medicare Benefit Policy Manual, (CMS Publication 100-02, Ch. 7) Medicare pays for care in a beneficiary’s home, when qualifying criteria are met, and documented.
As part of overall efforts to move Medicare payment away from fee for service and toward a structure that holds providers accountable for patient outcomes and costs, the Centers for Medicare and Medicaid Services (CMS) has made significant changes to the home health and skilled nursing facility (SNF) payment systems. The SNF Patient-Driven Payment Model (PDPM) began October 1 (the start of
29/10/2019 · The topics that will be discussed include: Medicare benefits, provider enrollment requirements, patient screening tools, new Medicare card, billing guidelines Part A and B, claim submission errors Part A and B, Medicare initiatives and explore the self-service tools and IHS Training Manual available on the Novitas website.
* dialysis billing manual medicare 2018 * provider reimbursement manual part 1 * what k codes of manual wheelchiars will medicare pay for * where are status indicators in cpt coding manual * wellmark 3m eapg definitions manual; Category: Medicare codes PDF. Tags: billing, health, home, manual, medicare
For additional information, refer to section 40.1 of the Medicare Claims Processing Manual (CMS Pub. 100-04, Ch. 10), or the Top Claim Submission Errors for Home Health Providers: Error 38107 web page.
Home health services must be billed on a CMS 1500 claim form. Institutional Billing Manual – South Dakota Department of Social … Managed Care and Health Home Updates.
Medicare Home Health Agency Manual – Medicare add
Home Health Part A – medicare b code
Home Health Care Billing and Reimbursement . Monday, April 29, 2019. The TRICARE benefit for home health care services closely follows Medicare’s Home Health Agency Prospective Payment System (HHA-PPS), which offers in-home therapies, social work services and part-time or intermittent skilled nursing services up to a maximum of 35 hours per week for eligible beneficiaries.
You can receive home health care coverage under either Medicare Part A or Part B.Under Part B, you are eligible for home health care if you are homebound and need skilled care.There is no prior hospital stay requirement for Part B coverage of home health care. There is also no deductible or coinsurance for Part B-covered home health care.
Medicare will review the information and cover the services if the services are medically necessary and meet Medicare requirements. Your Medicare home health services benefits aren’t changing and your access to home health services shouldn’t be delayed by the pre-claim review process. For more information, call us at 1-800-MEDICARE.
Processing Manual, Chapter 10, “Home Health Agency Billing,” §40.2, and 42 CFR. Medicare Benefit Policy Manual Chapter 10 – CMS. www.cms.gov. 10.3.9 – Transportation Requested by Home Health Agency. 10.3.10 … Processing Manual, Chapter 15, “Ambulance,” for instructions for processing ambulance. Medicare Claims Processing Manual
offered based on their location, budget and health care needs. Cigna Medicare Advantage Health Maintenance Organization (HMO) Plans: Customers are required to select a PCP and must receive all covered services by utilizing in-network providers, except in the case of emergency. Select service areas do not require the use of referrals. Please
Home Health Coverage Guidelines Medicare Benefit Policy Manual, (CMS Publication 100-02, Ch. 7) Medicare pays for care in a beneficiary’s home, when qualifying criteria are met, and documented.
Home Health Agency Manual – CMS. billing requirements for home health agencies (HHAs) under the home health … patient’s death, patients who are no longer eligible for Medicare home health, … Medicare Claims Processing Manual Chapter 10 – Home Health. 40 – Completion of Form CMS-1450 for Home Health Agency Billing … to the
Medicare Benefit Policy Manual Home – Centers for
Home Health Part A – medicare b code
You can receive home health care coverage under either Medicare Part A or Part B.Under Part B, you are eligible for home health care if you are homebound and need skilled care.There is no prior hospital stay requirement for Part B coverage of home health care. There is also no deductible or coinsurance for Part B-covered home health care.
Processing Manual, Chapter 10, “Home Health Agency Billing,” §40.2, and 42 CFR. Medicare Benefit Policy Manual Chapter 10 – CMS. www.cms.gov. 10.3.9 – Transportation Requested by Home Health Agency. 10.3.10 … Processing Manual, Chapter 15, “Ambulance,” for instructions for processing ambulance. Medicare Claims Processing Manual
Are home health visits covered? The FQHC must be authorized by CMS to provide home health visits. The only states that qualified at this time are Alaska and CMS IOM, Publication 100‐02, Medicare Benefit Policy Manual, Chapter 13, Section 90.4. 10. Is current procedural code 94664 billed in addition to the office visit code on the same date of
Home Health Outpatient Therapy Billing. Outpatient therapy services may be furnished by a home health agency (HHA) to individuals who are not homebound or otherwise are not receiving services under a home health plan of care (POC). These services are not paid under the Home Health Prospective Payment System (HH PPS).
Consolidated Billing • HHA must bill for all home health services which includes: – Nursing and therapy services – Routine and non-routine medical supplies – HH aide services – Medical social services • All home health services paid on a cost basis included in PPS rate • …
CMS IOM Publication 100-04, Medicare Claims Processing Manual, Chapter 12, Section 180; Related Articles. Noridian Medicare Portal (NMP) Offers Expanded Denial Details – Entitlement, Date of Death, Hospice, and Home Health; Certifying Patients for the Medicare Home Health Benefit – Revised SE1436
Home Health Services Billing Manual (F245-424-000) Below is a list of the billing manuals L&I provides: • General Provider Billing Manual. • CMS 1500 Billing Manual. • Home and Residential Care Billing Manual. Billing Manual – Nevada Medicaid. Feb 20, 2015 … manual. • Updated First Health Services mailing address. • Links to Internet
Coverage, billing and payment guidelines are found in the Medicare Claims Processing Manual, Chapter 18, “Preventive and Screening Services;” Chapter 17, “Drugs and Biologicals;” and the Medicare Benefit Policy Manual, Chapter 15, “Covered Medical and Other Health Services,” §50.4.4.2.
23/07/2018 · SNF overlapping with home health care: A patient cannot receive home health care while in a SNF regardless of whether the patient is under a Medicare Part A stay. The home health agency is required to omit dates of service from their claim while the patient is under the care of the SNF between the admit and discharge dates.
29/10/2019 · The topics that will be discussed include: Medicare benefits, provider enrollment requirements, patient screening tools, new Medicare card, billing guidelines Part A and B, claim submission errors Part A and B, Medicare initiatives and explore the self-service tools and IHS Training Manual available on the Novitas website.
Home A federal government website managed and paid for by the U.S. Centers for Medicare & Medicaid Services. 7500 Security Boulevard, Baltimore, MD 21244 CMS & HHS Websites [CMS Global Footer]
For additional information, refer to section 40.1 of the Medicare Claims Processing Manual (CMS Pub. 100-04, Ch. 10), or the Top Claim Submission Errors for Home Health Providers: Error 38107 web page.
Medicare Benefit Policy Manual Home – Centers for
Home Health Agency Billing Manual – medicare b code
See Figures 1.1 and 1.2 for examples of some billing job descriptions. Home Health Billing Overview A certified home health agency is authorized by the Centers for Medicare & Medicaid Services to accept Medicare and Medicaid reimbursement. Certified home health agencies must follow the Conditions of Participation 42 CFR 484 requirements.
medicare replacement plans billing guidelines for home health. PDF download: Medicare Benefit Policy Manual Chapter 7 – Home Health … – CMS. a home health plan of care since the law requires consolidated billing of ….. If a patient’s enrollment in a Medicare …
Medicaid Home Health Billing. PDF download: Medicare Claims Processing Manual – CMS.gov. www.cms.gov. Institutional providers, including home health agencies, use one of two institutional claim formats to bill Original Medicare. In the great majority of cases,
Home health services must be billed on a CMS 1500 claim form. Institutional Billing Manual – South Dakota Department of Social … Managed Care and Health Home Updates.
This seminar offers education and strategy to provide agency owners, administrators, business managers and billing staffs with practical information to equip your agency to collect the reimbursements due for payer sources. Home health payments continue to take a hit and episodic payments will be reduced in 2016. The 2% Sequestration is legislated through 2023.
offered based on their location, budget and health care needs. Cigna Medicare Advantage Health Maintenance Organization (HMO) Plans: Customers are required to select a PCP and must receive all covered services by utilizing in-network providers, except in the case of emergency. Select service areas do not require the use of referrals. Please
For additional information, refer to section 40.1 of the Medicare Claims Processing Manual (CMS Pub. 100-04, Ch. 10), or the Top Claim Submission Errors for Home Health Providers: Error 38107 web page.
Coverage, billing and payment guidelines are found in the Medicare Claims Processing Manual, Chapter 18, “Preventive and Screening Services;” Chapter 17, “Drugs and Biologicals;” and the Medicare Benefit Policy Manual, Chapter 15, “Covered Medical and Other Health Services,” §50.4.4.2.
Home Health Outpatient Therapy Billing. Outpatient therapy services may be furnished by a home health agency (HHA) to individuals who are not homebound or otherwise are not receiving services under a home health plan of care (POC). These services are not paid under the Home Health Prospective Payment System (HH PPS).
Home Health Agency Manual – CMS. billing requirements for home health agencies (HHAs) under the home health … patient’s death, patients who are no longer eligible for Medicare home health, … Medicare Claims Processing Manual Chapter 10 – Home Health. 40 – Completion of Form CMS-1450 for Home Health Agency Billing … to the
Payment for rehabilitation therapy services provided by home health agencies … Medicare and Home Health Care – Medicare.gov. about Medicare home health care benefits for people with Original Medicare. This booklet has important information about the following: Who is eligible. . Medicare Claims Processing Manual – CMS
Home health care; 2 ways to find out if Medicare covers what you need. Talk to your doctor or other health care provider about why you need certain services or supplies. Ask if Medicare will cover them. You may need something that’s usually covered but your provider thinks that Medicare won’t cover it …
Home Health Medicare Manual – medicare b code
This seminar offers education and strategy to provide agency owners, administrators, business managers and billing staffs with practical information to equip your agency to collect the reimbursements due for payer sources. Home health payments continue to take a hit and episodic payments will be reduced in 2016. The 2% Sequestration is legislated through 2023.
Home Health Medicare Billing Codes Sheet
NOTE Should you have landed here as a result of a search
Changes to Physician Documentation Requirements for Home
Medicare Home Health Agency Billing. PDF download: Medicare Claims Processing Manual Chapter 10 – Home Health. http://www.cms.gov. HHPPS Episode File. 40 – Completion of Form CMS-1450 for Home Health Agency Billing. 40.1 – Request for Anticipated Payment (RAP). 40.2 – HH PPS Claims. Medicare Home Health Benefit – CMS. http://www.cms.gov
medicare replacement plans billing guidelines for home health
Getting Started with Home Health Billing Guide
Home Health Services Billing Manual (F245-424-000) Below is a list of the billing manuals L&I provides: • General Provider Billing Manual. • CMS 1500 Billing Manual. • Home and Residential Care Billing Manual. Billing Manual – Nevada Medicaid. Feb 20, 2015 … manual. • Updated First Health Services mailing address. • Links to Internet
Medicaid Home Health Billing – Medicare PDF List
Home Health Billing & Reimbursement
30/04/2019 · Changes to Physician Documentation Requirements for Home Health Care. Dear Colleague: Medicare has changed the physician documentation requirements for certification of home health care for dates of service effective January 1, 2015.
medicare replacement plans billing guidelines for home health
Home Health Part A – medicare b code
Home Health Care Billing and Reimbursement . Monday, April 29, 2019. The TRICARE benefit for home health care services closely follows Medicare’s Home Health Agency Prospective Payment System (HHA-PPS), which offers in-home therapies, social work services and part-time or intermittent skilled nursing services up to a maximum of 35 hours per week for eligible beneficiaries.
Home Health Medicare Manual – medicare b code
Medicare Home Health Billing Training – Medicare Training
Medicare Advantage (MA) Plans — Claim Filing Tips When A Beneficiary Receiving Home Health Services Enrolls / Disenrolls. When a beneficiary is enrolled in an MA plan, the home health services provided during their enrollment period must be submitted and processed by the MA plan, not the Medicare Administrative Contractor (MAC) like CGS.
Medicaid Home Health Billing – Medicare PDF List
Changes to Physician Documentation Requirements for Home
Home Health Coverage Guidelines
CMS IOM Publication 100-04, Medicare Claims Processing Manual, Chapter 12, Section 180; Related Articles. Noridian Medicare Portal (NMP) Offers Expanded Denial Details – Entitlement, Date of Death, Hospice, and Home Health; Certifying Patients for the Medicare Home Health Benefit – Revised SE1436
Medicare Advantage (MA) Plans — Claim Filing Tips When A
Home A federal government website managed and paid for by the U.S. Centers for Medicare & Medicaid Services. 7500 Security Boulevard, Baltimore, MD 21244 CMS & HHS Websites [CMS Global Footer]
Home Health Medicare Manual – medicare b code
Home Health Medicare Billing Manual – medicare b code
For additional information, refer to section 40.1 of the Medicare Claims Processing Manual (CMS Pub. 100-04, Ch. 10), or the Top Claim Submission Errors for Home Health Providers: Error 38107 web page.
Home Health Agency Billing Manual – medicare b code
Home Health Coverage Guidelines
Home Health Agency Manual – CMS. billing requirements for home health agencies (HHAs) under the home health … patient’s death, patients who are no longer eligible for Medicare home health, … Medicare Claims Processing Manual Chapter 10 – Home Health. 40 – Completion of Form CMS-1450 for Home Health Agency Billing … to the
Medicare Payment and Policies for Home Health
Home health services must be billed on a CMS 1500 claim form. Institutional Billing Manual – South Dakota Department of Social … Managed Care and Health Home Updates.
medicare replacement plans billing guidelines for home health
Medicare Home Health Billing Training – Medicare Training